This is the last in a series of five articles in which Michael Settas elaborates on the critically important distinction between universal health coverage (a policy objective) and the proposed National Health Insurance (a financing mechanism). He provides a high-level background to the country’s two major health assets, the private and public sectors, as well as a history of health policy since 1994 that has culminated in the contentious and now imminent National Health Insurance proposal. You can read the first, second, third, and fourth articles here, here, here, and here.
The modern democratic era has witnessed a health policy process with a variety of inquiries, new health proposals, and new legislation, although broadly speaking it can ideologically be split into two eras, the first from 1994 to 2007 and then from 2008 onwards.
Unlike where the overall economic performance of the country was distinctly different between the above two periods, health policy has had mixed experiences of ups and downs throughout both periods, ranging from realism, pragmatism, some fanciful thinking, to sheer lunacy!
1994 to 2007
Two policies that were reasonably well grounded in realistic pragmatism were the introduction of the new Medical Schemes Act in 1998 and the Taylor Committee recommendations of the early 2000s.
Prior to the transition to the democratic era, the former National Party Health Minister, Rina Venter, introduced an amendment to the then Medical Schemes Act in 1989, paving the way towards a risk-rated medical scheme environment. This allowed medical schemes to operate more like life insurers, where cover could be declined in the case of bad risks and only good risks brought in – an underwriting practice known as ‘cherry picking’.
These new laws were not widely utilised by incumbents, in an industry that was by then rather stale and lacking in innovation. Nonetheless, they were used by some new entrants and there was obviously scope for an industry-wide shift to using the new laws, which would have excluded high-risk and vulnerable groups from private coverage. This would then have removed the medical schemes industry from being a vital component of a universal health coverage framework for the country.
The industry also had many other weaknesses, such as light and ineffective regulation, resulting in poor governance and a misalignment of interests between stakeholders, which resulted in many abuses of consumers and medical scheme funds.
The reversal to a non-risk-rated environment came in the form of the new Medical Schemes Act (MSA), of 1998. This cemented the social solidarity framework outlined in my previous article but also, importantly, it substantially enhanced the powers of the new regulator, the Council for Medical Schemes. The one substantial shortcoming of the new MSA was the removal in the implementation phase of any form of mandatory membership, which has contributed to the cost spiral witnessed in the industry over the past two decades.
Nonetheless, as the Health Market Inquiry (HMI) emphasised, this shortcoming in the regulatory framework could have been addressed with appropriate regulatory amendments. Sadly this has not happened. So, although the design of the private sector is fully supportive of and constitutes a functional component of a universal health coverage framework in the country, the now excessive cost limits its ability to expand coverage to more citizens.
Implementation of the recommendations of the HMI is urgently required.
Taylor Committee
The final Taylor Committee proposal of the early 2000s was made after extensive investigation into a comprehensive social security system for the country, of which one component was findings and recommendations on sustainability enhancements to the overall health framework in South Africa, across both the public and private sectors.
The final health proposals involved the establishment of a new state-sponsored medical scheme that would fund the cost of care in public facilities for citizens in the lower income categories and informal sector. The state medical scheme would be a contributory scheme, with mandatory membership. All medical schemes were required to include income-based contribution tables to enhance cross-subsidy from higher to lower income earners. Nonetheless, the contributory nature was seen as a tax by labour unions and the proposal was rejected by most of them.
Importantly, the Taylor structure meant that the public sector received two additional sources of funding over and above that provided through general taxes: firstly from the state medical scheme and secondly from private medical schemes where they would contract with the public sector for medical services. This would also bring about much-needed competition between the two sectors and serve to place pressure on both to improve efficiencies and quality.
Summary of Taylor Commission Health Proposals (2003)
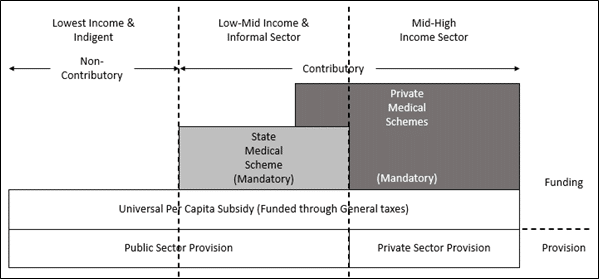
The Taylor proposal represented a financially realistic solution to improving the ‘depth’ of universal health coverage in the country, in fairly stark contrast to the populist and unrealistic proposal of ‘free and comprehensive’ healthcare for all, as proposed by the NHI.
AIDS Denialism
Almost without doubt, the most damaging policy era in South Africa’s history was former President Thabo Mbeki’s lunacy of denying that HIV caused AIDS. In 2000 he convened a Presidential Advisory Panel, which included certain scientists who supported this claim that HIV did not cause AIDS.
Mbeki appointed the late Manto Tshabalala-Msimang as health minister, who further propelled Mbeki’s denials and promoted the use of unproven remedies such as beetroot, garlic, and lemon juice to treat AIDS – leading to her acquiring the moniker, ‘Dr Beetroot’. Many public sector doctors were also dismissed for ‘illegally’ prescribing anti-retroviral drugs to AIDS patients.
This stance has been blamed for the preventable deaths of more than 300 000 people in South Africa, and severely delayed the introduction of anti-retroviral drugs for millions of infected patients. It also sowed confusion amongst the general populace about practising infection prevention measures.
Fortunately, in 2008 after Kgalema Motlanthe took up the presidency, Barbara Hogan was appointed health minister. She declared, “The era of denialism is over completely in South Africa“. Since then, South Africa has gone on to create the world’s largest HIV management programme, with current estimates of more than 5 million participants.
2008 Onwards – National Health Insurance
After Thabo Mbeki was ousted as president in 2008, the more left-leaning members within the tripartite alliance voiced their preference for the development of National Health Insurance (NHI). In particular, the proposals that had been put forward earlier by the Taylor Committee were despised, as these did not fit into the populism that espoused ‘free healthcare’. Predictably, the Taylor proposal was officially shelved as policy in exchange for NHI at the ANC’s elective conference in December 2007!
In 2009, the then Minister of Health, Aaron Motsoaledi, established a Ministerial Advisory Committee (MAC) to guide and establish policy on development of the NHI proposal. This led to the publication of the NHI green paper in 2011 and two further white papers in 2015 and 2017. In 2018, a draft NHI Bill was published, and the final Bill was accepted by Cabinet in August 2019.
As outlined in my first article in this series, the NHI is a very high-risk proposal. The policy process has been characterised by an obtuse focus on the centralisation of the funding of both the private and public sectors – into a national monopoly single-payer called the NHI Fund (NHIF), which has been heavily touted by government officials as being a ‘silver bullet’ that will magically resolve all the country’s healthcare problems.
The rhetoric and bluster from health officials tells you that the NHI is long on ideology and extremely short on pragmatic realism! The following are key points of failure in the policy process that have largely characterised the development of NHI:
- A lack of clarity on the rationale for the proposal, i.e. clarity on the problem statement that motivates for NHI. As was outlined in Article One, NHI argues for the need of an existing attribute of the health system, i.e. universal health coverage. It also argues that the state has declining resources – Article Two in the series clearly demonstrates that the public sector’s financial and human resources have improved substantially over the past two decades. Lastly, it argues by extension of the resource argument, that the existence of the private sector is also causal to the public sector problems, which remains a factually unfounded argument.
- A virtual absence of technical and feasibility analyses, despite the Ministerial Advisory Committee having been in place for ten years since 2009. This is an extremely concerning aspect of this proposal – in fact we can regard it as reckless to contemplate the wholesale and simultaneous disruption of two very substantial sectors of the country when there is such a dearth of analyses supporting it. But even if more comprehensive analyses had been performed, it is also plausible that the magnitude of the NHI proposals are such that it remains unlikely that any in-depth analyses will uncover all potential unforeseen and unintended consequences. This is what makes this such a very high-risk proposal.
- The complete absence of a detailed technical costing analysis. The revenue ‘target’ of 8.5% of GDP within the policy papers makes the NHI an extreme outlier for a developing economy. Even prior to the economic devastation wrought by the Covid-19 lockdown, the economy suffers from a number of structural growth-inhibiting impediments, which makes the raising of additional NHI taxes equivalent to 3% of GDP (± R165bn in 2021 values) entirely unfeasible. It furthermore also argues against evidence produced by National Treasury and the Davis Tax Committee that NHI is wholly unaffordable under current circumstances.
- Against the backdrop of the disturbing findings of the Zondo Commission, the very weak governance framework outlined in the NHI Bill creates a strong likelihood that it has intentionally been designed in this way. There is an overt concentration of authority in the hands of the Minister of Health to control all appointments to the board of the NHI Fund as well as all of its various sub-committees. There is little oversight of this authority, with minimal checks and balances on decisions or any separation of vested powers, which, combined with the centralised and monopolised nature of the NHI proposal makes this the purest recipe imaginable for endemic corruption and the further fostering of the entrenched patronage networks within the ANC.
In Article Two I outlined how – at 11% of GDP – Cuba was such an extreme outlier in public healthcare expenditure for an upper-middle income country. Cuba has a nationalised and monopolised health system, similar to the NHI proposal. It is well known that the ANC is enamoured with the euphemistically termed developmental ‘achievements’ of Cuba, with officials often waxing lyrical about what an exemplar the communist country is.
“Cubans are suggesting that Africans, and South Africans in particular, must be focused to get rid of the remnants of colonialism and reject imperialist thinking as propagated by institutions such as the World Bank and the International Monetary Fund. If anything, Cubans are entreating us to make sure that the economy is in the hands of the people and that we must push for radical economic transformation that will deliver an inclusive economy.”
The Late Jessie Duarte – SA, Cuba, and our principled alliance – November 2019
In the ANC’s presentation to the parliament’s Health Portfolio Committee in February 2022, it extends this infatuation, categorically stating it wants to copy the Cuban health system:
“The best national health system, health service delivery and funding mechanism with excellent outcomes is that of Cuba.”
Cuba is an extreme outlier in health system design, one component of which is a massive oversupply of doctors who are often ‘trafficked’ to other countries with doctor shortages. This trafficking often occurs along with gross violation of the human rights of these doctors, with much more interest being shown for the Cuban government’s coffers (and corrupt public officials) than the affected medical personnel.
Cuba does attain good clinical outcomes in contrast to many other developing economies, such as South Africa. But these outcomes are skewed when contrasted against cost. There are a number of other upper-middle income countries that achieve similar outcomes to Cuba, but at a substantially lower cost than the communist Cuban health system.
The cost of the Cuban health system is further exacerbated when considering two additional factors. Firstly, Cuban doctors get paid very low salaries, with many leaving their vocations to take up jobs as taxi drivers or tour operators, where they are able to earn substantially better incomes. Consider that of South Africa’s total public health expenditure in 2020/21, 60% was on employee compensation.
Secondly, Cuba is somewhat of an anomaly for a developing economy, with a very low population growth over the past two decades (<2%). Considering these ameliorating factors, it is quite a wonder how Cuba still manages to incur such a high health expenditure, at 11% of GDP.
In my opinion, it reflects the standard deficiencies of monopolies – most especially public ones. Similar to the NHI proposal – and very much like Eskom, to which many South Africans can relate.
Where to Now?
The presidency of Jacob Zuma has been euphemistically termed the “lost decade”, but in terms of the health department we can talk of two lost decades. Little policy adjustment was made during this time, as the earlier major reform policy, the Taylor Committee, was side-lined after President Thabo Mbeki was eventually ousted by those opposing his so-called “neo-liberal” economic policies. Subsequent to this period, and very much like in the Eskom disaster, the Department of Health seized upon an unworkable, ideologically appealing policy, the NHI. It would not be too much of a stretch to call the NHI a non-policy.
Officially it is now 13 years old, with very little to show in the way of how exactly it will better serve South Africans. In the meantime, the health department became a plundering pot for unqualified cadres and an expanding patronage network creating a feeding frenzy off bloated and ill-informed supply contracts across the department.
The widespread and rapidly constituted fraud that pervaded the awarding of contracts for distribution of personal protection equipment (PPE) in the early part of the Covid-19 pandemic serves as a stark reminder of how well-entrenched and opportunistic these patronage networks are within the health department. The final report from the Special Investigating Unit (SIU) on PPE fraud has recommended prosecutions for nearly 3 000 PPE contracts – and this was only for Covid-19 expenditure between April and September 2020!
The horrific assassination last year of Babita Deokaran, a whistle-blower within the health department, is a tragic but highly informative example on this point. She not only blew the whistle on malfeasance within the department but was willing to stand as a key witness in a multi-million-rand fraud investigation on Covid-19 PPE tenders.
An initial confession from one of the six apprehended suspects charged with Deokaran’s murder indicated that former health minister, Zweli Mkhize, was implicated in the assassination. The suspect has subsequently withdrawn his confession, claiming it was obtained under coercion, so the question of who ordered the hit remains unanswered.
This amply informs us that there are no limits to the depraved lows perpetrators will descend to in protecting themselves from prosecution. These cannot be regarded as the actions of any legitimate government, but rather of a predatory criminal network.
All these factors warn us to be highly suspicious of policies proposed by the ANC that – like the NHI – have almost exclusively focused on concentrating authority and influence over a massive, centralised pool of public funds. Virtually nothing else has been focused on during this NHI policy process. In-depth technical and feasibility assessments should have been a focused and integral part of such a policy process – but it has not been so. Against which, suspicion should grow even further!
If South Africa is to fix the problems inherent in both the public and private health sectors, the NHI will come nowhere close to achieving them. It is obvious that better-researched, more pragmatic, and realistic policies are necessary and, importantly, drawn from an altruistic perspective.
But that remains highly unlikely while the country is under the grip of a ruling party that dispenses patronage and entrenches corruption above all else.
Let’s hope that grip is slipping – the signs are strong that it is. And a country awaits its right to enjoy its Section 27 constitutional rights.
The views of the writer are not necessarily the views of the Daily Friend or the IRR
If you like what you have just read, support the Daily Friend