This is the third in a series of five articles in which Michael Settas elaborates on the critically important distinction between universal health coverage (a policy objective) and the proposed National Health Insurance (a financing mechanism). He provides a high-level background to the country’s two major health assets, the private and public sectors, as well as a history of health policy since 1994 that has culminated in the contentious and now imminent National Health Insurance proposal. You can read the first and second articles here and here.
In 2013, the health department established the Office of Health Standards Compliance (OHSC), a body that routinely measures compliance by public health establishments against best practice clinical and management standards.
One could consider the OHSC to be analogous to a ‘clinical’ Auditor General, but it is not a Chapter 9 institution as it is appointed by and reports directly to the Minister of Health (although the OHSC describes itself as an independent body).
This lack of independence has been highlighted as a potential governance problem under NHI, as political pressure may be applied to influence achieving compliance, which is required for health facilities to contract with and hence earn revenue from the NHI Fund. The NHI Bill states categorically that only facilities (public or private) that achieve compliance status with the OHSC will be permitted to contract with the NHI Fund.
Nonetheless, the OHSC has conducted four inspection rounds on public facilities and all paint a grim picture. The OHSC’s reporting standard is based on 13 criteria and the two lowest overall scores in the 2018/19 report are for Leadership & Governance (22%) and Operational Management (35%). This likely prompted the then acting chair, Ms Oaitse Montshiwa, to note the following in her foreword of the report:
“The gaps identified in inspected HEs [health establishments] during 2018/19 were similar to findings in previous financial years, such as, lack of effective governance structures in the majority of inspected HEs. This impacted negatively on leadership as there was no evidence of oversight and/or accountability.”
This is a rather damning statement, but when examining the compliance outcomes in Table 1, it is obvious that it is entirely appropriate. The collective scores achieved by the 730 public health establishments inspected in this inspection report are shown below.
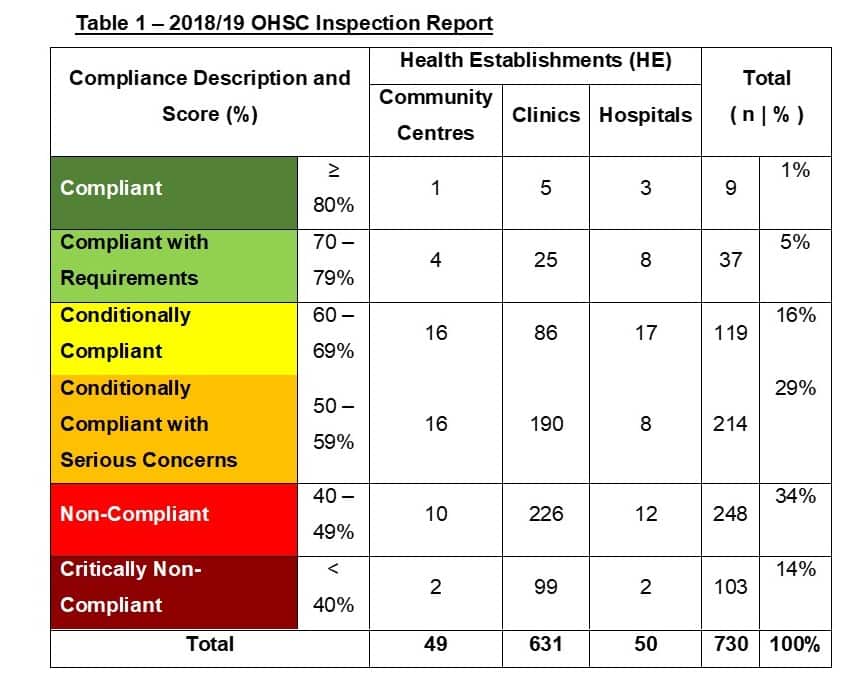
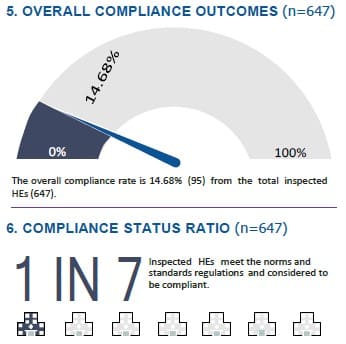
In the latest 2019/20 report, the compliance categories and the qualifying criteria have been substantially changed from those used in the previous three reports (as per Table 1 above), so a comparison with earlier reports is not possible. Nonetheless, the image below is an extract from the 2019/20 report summary, indicating that just under 15% of the 647 health entities that were inspected attained compliance status. In two provinces – Limpopo and North West – the compliance rates were zero.
In reference to the NHI proposal, it remains unclear how government proposes implementing NHI when such a small proportion of public facilities meet the compliance standard that is required in order to be accredited with the NHI.
It also raises a pertinent question! Since funding through the provinces will be removed under NHI, requiring that each and every facility derives its funding by contracting with the NHI Fund, what will happen to those facilities that fail compliance and hence accreditation? How will they operate? How will their staff get paid? How will citizens living in the regions they operate access medical care?
These sorts of questions remain unanswered!
It is very clear from these inspections that the vast majority of public facilities have a very long way to go in achieving better clinical and management standards, let alone being operationally capable of incorporating the additional administration functions – amongst others ‘billing-per-service-provided’ – that will be required under NHI.
This adds further credence to the NHI being politically motivated, as any rational observer must conclude that, under these circumstances, NHI is an irrational and unworkable policy, and that the health department’s focus should rather be on improving clinical and management standards substantially and sustainably.
Provincial Comparison
Poor health outcomes are reflected in the medicolegal claims against the provinces. Table 2 shows budgets, filled posts, hospital beds, medicolegal liabilities and maternal mortality rates (MMR) per province.
The provincial equitable share formula normalises per capita budgets on a reasonably equitable basis, although the Limpopo, Mpumalanga and North West budgets are somewhat below the national average.
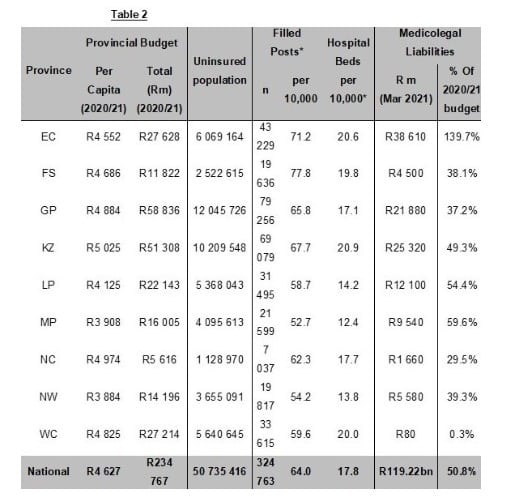
The number of personnel and hospital beds per 10,000 uninsured citizens show somewhat more variance across provinces than their per capita budgets, although these factors are determined by the provinces. There can also be greater variances between provinces in medical provider densities of specific disciplines, which are driven by structural features. For example, the density of medical specialists will be highest in provinces with the most tertiary and central hospital beds.
As can be seen above, the latest financials show that the state had a medicolegal liability of nearly R120bn as at 31 March 2021. There have been no meaningful measures proposed to manage this gargantuan liability, save for a request by the Minister of Justice in 2017 to the SA Law Reform Commission to undertake research on the matter and offer recommendations. This resulted in a paper that mainly dealt with legal aspects of the rise in medical malpractice liability claims and possible legal solutions to dealing with them, but there is no focused attention on avoiding liability by improving the quality of care delivered.
Recently, President Ramaphosa announced that he had instructed the Special Investigating Unit (SIU) to discover fraudulent medicolegal claims against the state. While this is a step in the right direction, it again points to a dysfunction within the public sector, where such nefarious activities are enabled. It would be naïve to believe that all medicolegal cases against the state are entirely legitimate, but in many cases they are either not defended or the defence lacks any vigour, thus leaving the state exposed unnecessarily to this growing liability.
Medicolegal liability provisions have similar attributes to government borrowings in that they are not payable immediately, but once they amass to these levels, they can threaten the country’s long-term financial stability. If the current national trend continues, this liability will be over R200bn by 2024/25, which I estimate will equate to around 75% of the DoH’s entire annual budget.
Unless the health department can address the poor quality of care in the public sector and the levels of corruption and cadre deployment that hamper proper management, these growing liabilities will massively undermine the state’s ability to improve healthcare. Sadly, this has become a vicious cycle, as one failing (exposure to liability) leads to the other failing (poor quality healthcare) which leads to further liability and so on and so forth.
In terms of the proxy performance indicators in Table 2 above, namely maternal mortality rates and medicolegal liabilities, the Western Cape is clearly an outlier among the provinces, even though it has similar financial, human and facility resources to the other provinces. The Western Cape’s medicolegal liability is a comparatively insignificant R80m, equating to only 0.3% of the province’s budget, whereas for the rest of the provinces the liability equates to 57% of their combined budgets.
In an expert review of the NHI proposal by Professor van den Heever, a health economist from Wits University, he confirms that maternal mortality rates (MMR) are generally accepted as a proxy indicator for institutional management performance.
The Western Cape’s substantially superior outcomes in MMR, along with their insignificant medicolegal claims, provides a clear indicator that with better management and governance, significantly improved outcomes are possible in the other provinces ‘within their current resource allocations’.
Summary
The above overview provides a clear picture that public sector performance should be considerably better.
Outcomes and quality are clearly not where they should be and the reports from the OHSC provide a strong indication that the key problems are a lack of proper governance structures, poor management of facilities and accountability. The Auditor General’s findings on the health department corroborate the findings of the OHSC, also routinely highlighting governance failures and poor management capabilities.
“The country’s health services are in crisis!”
Kimi Makwetu, The late Auditor General, 2019
I showed in article 2 that public sector expenditure has been growing substantially in both real and per capita terms for the past two decades and we compare favourably in public expenditure with other upper middle-income countries. The number of medical personnel employed by the state also increased very substantially during this period.
The Western Cape is the only province in the country governed by the Democratic Alliance, and evidence suggests that they have been able to contain corruption and cadre deployment to a far greater degree than the ANC, and hence maintain better governance frameworks and retention of qualified managers within their health facilities. This more likely explains their substantially better performance on maternal mortality rates and comparatively non-existent medicolegal liabilities.
This is a strong indicator that the poor performances of the other provinces are caused more by institutional management failures, poor governance and the resultant malfeasance rather than from an insufficiency of funding or personnel.
In the next article, I delve into the private health sector.
[Image: https://pixabay.com/photos/medical-equipment-medicine-4099429/]
The views of the writer are not necessarily the views of the Daily Friend or the IRR
If you like what you have just read, support the Daily Friend